“I have recently been experiencing pain in the side of my hip since starting to exercise more again. I can’t lie on either side at night and it hurts when I try to run or stand for too long, or if I try to hold my 2-year-old son on my hip. It even hurts after resting when I get up from sitting at my desk for long periods of time. My Doctor says I have ‘Trochanteric Bursitis’ - how do I fix it?”
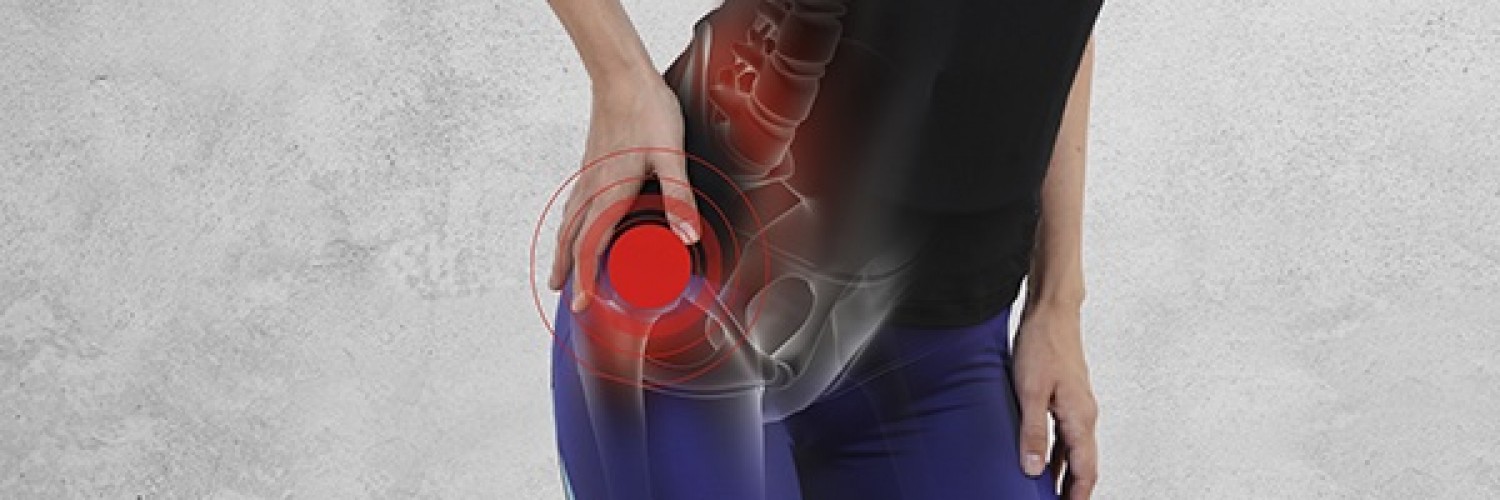
There are a number of conditions in the back, hip, and pelvic area that can present as pain or discomfort in the side of the hip, which is why a thorough clinical assessment is required to rule out lumbar spine, nerve, and hip joint injuries.
Pain in the side of the hip is commonly a result of gluteal muscle irritation or injury rather than trochanteric bursitis alone. This is known as Gluteal Tendinopathy, often labelled broadly as ‘Greater Trochanteric Pain Syndrome’. Bursitis is irritation of the cushioning under the tendon, and will often occur as a consequence of tendon injury and continue to be aggravated by compression over the area. In those with Gluteal Tendinopathy, activities such as lying on your side (both painful and non-painful side), stairs, walking, and sitting compress the tendons and bursae and cause these structures to become irritated and painful.
Gluteal Tendinopathy is most common in women aged 35-65+ years old, but is also seen frequently in men and women of all age groups who are either sedentary or active. Often it occurs when you return to activity after a period of deconditioning, and those with weaker gluteal muscles, high BMI, or hormonal changes (eg. menopause) are at higher risk of this condition.
Management of Gluteal Tendinopathy is largely dependent on load modification, where the below do’s and don’t’s can be very helpful in reducing those aggravating compressive loads.
DO:
- Sleep on your unaffected side with a pillow between your knees
- Modify your exercise load guided by your Physiotherapist
- Sit in higher positions with your knees slightly below your hips
DON’T:
- Stand on one leg/hip hitch
- Cross your legs
- Foam roll directly over the tendon or stretch the affected glute
Other strategies such as dry needling, massage, and adjusting foot posture/support are beneficial in the early stages of rehab. A supervised, therapeutic exercise program is essential to gradually re-load the gluteal muscles and carefully strengthen your hips and core. Cortisone injections to the bursa are recommended in some cases to help with pain and assist in facilitating rehabilitation, but they are not a cure for Gluteal Tendinopathy and multiple injections into the tendon are not recommended. A Physiotherapist will help you with specific evidence-based exercises, advice, and treatment to get you back to your best and kick your Gluteal Tendinopathy in the butt!