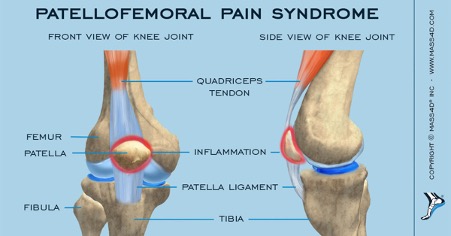
Patellofemoral Pain Syndrome (PFPS) refers to a multifactorial pathogenesis that leads to pain in and around the patella in the absence of other pathology. Historically, it has been referred to as anterior knee pain and is extremely common throughout the lifespan. Almost anyone can get it, but it particularly affects runners, cyclists, hikers, gym-goers, and office workers.
Clinical Features
- Pain under and around the patella
- Aggravated by activities that increase PFJ compressive forces e.g., squatting, prolonged sitting with knees bent, wearing high heels, lunges, ascending/descending stairs.
- Crepitus or crunching sounds when you bend and straighten your knee
- Pain related to a change in activity levels
- Tenderness on medial or lateral aspect of patella
- Restricted PFJ movements.
Are investigations required?
Generally, investigations are not required to make a diagnosis of PFPS.
Causes
PFPS is initiated by increased training loads or unaccustomed activity that overloads the patellofemoral joint (PFJ). Increased training loads can occur from changes in training volume, frequency, repetitions, intensity, or training surfaces. See below for contributing factors that influence PFJ load:
- Weakness in the quadriceps
- When the quadriceps are weak, specifically the VMO, the vastus lateralis can exert higher forces resulting in a lateral glide, tilt or rotation of the patella. Therefore, when the knee straightens and bends, the patella won’t track correctly in the groove, leading to pain particularly on the lateral facet.
Tight iliotibial band (IT band)
- A tight IT band pulls the patella laterally placing excessive lateral force on the patella.
Weakness of hip muscles
- Weakness in the hip external rotators (glutes) results in compensatory foot pronation, overloading the knee joint medially.
Tight calf muscle
- Can lead to compensatory foot pronation and increase the posterior force on the knee
Patella orientation and alignment
- Various patella orientations may lead to changes in how the patella tracks and thus, can cause overuse/overload leading to irritation of soft tissues. Similarly, long-term deviation of patella alignment and orientation leads to muscular imbalances or biomechanical abnormalities which further provokes PFPS.
Foot pronation
- Foot pronation (foot rolls inwards) causes compensatory internal rotation of the tibia during the weight acceptance phase of walking, which prevents the tibia from fully externally rotating during midstance. This prevents the knee from completely locking and causes the femur to compensate, increasing the contact pressure between the patella and lateral trochlear groove. This increases bone stress and symptoms of PFPS.
- Weakness in the hip muscles and tight IT band can further contribute to foot pronation.
Q-Angle
- A q-angle refers to the angle formed between the quadriceps muscle and patella tendon i.e., the amount of knee bend/valgus. A angle greater than 18-20 degrees could indicate patella tracking problems. Females tend to have greater Q-angles due to wide hips.
Neuromuscular Control
- Control of the VMO is assessed to identify if the muscles are contracting at the right time. When the muscle does not fire when needed, it increases the risk of PFJ overload.
Initial Treatment
- Pain management
- Rest from aggravating activity
- Ice
- Anti-inflammatory as needed
- Pain-free isometric home exercises. Isometric exercises can be implemented in the early phase of management. It is advantageous as it minimizes the stress on the PFJ while targeting the quadricep muscle/VMO. An example of this is called “Quads over fulcrum”
- Modified exercise as prescribed by your physiotherapist
Manual therapy
- Your physiotherapist will decide what the optimal treatment plan will be based off their objective and subjective assessment. Commonly, soft tissue, dry needling and patella mobilizations are effective in easing symptoms
Taping
- Patella taping should have an immediate pain-relieving effect. This technique can be used as an interim measure to relieve symptoms whilst other contributing factors are being corrected.
Exercise therapy
- The mainstay treatment is a specific progressive strengthening program consisting of exercises to improve quadriceps and hip muscle activation and strength, core strength and motor control of the whole lower limb kinetic chain. Here at Evado Studios, your physiotherapist might recommend an individualized Clinical Pilates or Clinical Strength training program that is closely monitored by us.
- Proprioception exercises. An example of this Is single leg balance work.
Foam rolling
- Between your physiotherapist appointments, it would be advantageous to foam roll your lower limb muscles. In general, rolling is a simple self-manual therapy technique used to improve flexibility, mobility, recovery and athletic performance. TIP: if traditional foam rolling is too hard consider purchasing a massage gun.
Prognosis
Average recovery time is 1-2 months for a full injury resolution.
By Katrina Laczoffy
DPT, BExSpSc(Hons)
APA Physiotherapist, Evado Studios Hawthorn & Clayton
Click on the images below to expand.